A confluence of topics dealing with mental health, substance abuse, health, public health, Social Work, education, politics, the humanities, and spirituality at the micro, mezzo, and macro levels. In short, this blog is devoted to the improvement of the quality of life of human beings in the universe.
Saturday, March 24, 2018
Thursday, March 22, 2018
Sunday, March 18, 2018
Psychotherapy Stories podcast, Episode #1, Overview
Psychotherapy Stories podcast. Episode #1 - Overview of the podcast with description of purpose, mission, vision, goals, activities, resources, and evaluation.
Saturday, December 9, 2017
Substance abuse prevention programs work
This is an interesting video of how Iceland engaged in substance abuse prevention with its teenagers. The same type of programs have been developed and implemented in the United States.
The Genesee Council on Alcoholism and Substance Abuse (GCASA) developed and implemented a Drug Free Communities Coalition in the 2000s. It won the national CADCA award in 2006 for having the best Drug Free Communities Coalition in the United States.
The Drug Free Communities coalition was led at GCASA by Maryann Bowman, Shannon Ford, and Tom Talbot.
The Genesee Council on Alcoholism and Substance Abuse (GCASA) developed and implemented a Drug Free Communities Coalition in the 2000s. It won the national CADCA award in 2006 for having the best Drug Free Communities Coalition in the United States.
The Drug Free Communities coalition was led at GCASA by Maryann Bowman, Shannon Ford, and Tom Talbot.
Friday, December 8, 2017
People with psychiatric illness more stigmatized by the health care system than by the public at large
Sisti says the stigma around mental health is "systematized" in our health care system, more so than in the public view.
Health care providers are "rather leery about these individuals because these people are, often at least according to the stereotype, high-cost patients who maybe are difficult to treat or noncompliant," he says. "I think the stigma that we should be really focused on and worried about actually emerges out of our health care system more than from the public."
For more click here.
Thursday, December 7, 2017
People with serious psychiatric problems now cared for in the criminal justice system
From NPR 11/30/17
"Many times individuals who really do require intensive psychiatric care find themselves homeless or more and more in prison," Sisti says. "Much of our mental health care now for individuals with serious mental illness has been shifted to correctional facilities."
The percentage of people with serious mental illness in prisons rose from .7 percent in 1880 to 21 percent in 2005, according to the Center for Prisoner Health and Human Rights.
Many of the private mental health hospitals still in operation do not accept insurance and can cost upwards of $30,000 per month, Sisti says. For many low-income patients, Medicaid is the only path to mental health care, but a provision in the law prevents the federal government from paying for long-term care in an institution.
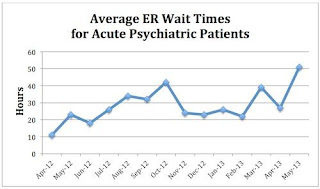
As a result, many people who experience a serious mental health crisis end up in the emergency room. According to data from the National Hospital Ambulatory Medical Care Survey, between 2001 and 2011, 6 percent of all emergency department patients had a psychiatric condition. Nearly 11 percent of those patients require transfer to another facility, but there are often no beds available.
"We are the wrong site for these patients," Dr. Thomas Chun, an associate professor of emergency medicine and pediatrics at Brown University, told NPR last year. "Our crazy, chaotic environment is not a good place for them."
For more click here.
Wednesday, December 6, 2017
Lack of psychiatric beds not the problem. Lack of funds for outpatient services is.
NPR has an interesting story about how the loss of psychiatric beds due to the era of deinstituionalization has led to a "mental health crisis" in the U.S. with people with psychiatric problems winding up in emergency rooms and prisons and jails.
The problem is not the lack of psychiatric hospital beds but the lack of outpatient services which has occurred because of a lack of funding. Health insurance payment systems for psychiatric disorders have led to difficulty accessing services with fewer providers available and people with problems winding up by default in other social systems whether it is criminal justice, social welfare, and health care services not equipped to manage people with mental illness.
For more on the NPR story click here.
The problem is not the lack of psychiatric hospital beds but the lack of outpatient services which has occurred because of a lack of funding. Health insurance payment systems for psychiatric disorders have led to difficulty accessing services with fewer providers available and people with problems winding up by default in other social systems whether it is criminal justice, social welfare, and health care services not equipped to manage people with mental illness.
For more on the NPR story click here.
Subscribe to:
Posts (Atom)